

Partnering for a Healthy Tomorrow
2024 Annual Report
When communities thrive, children flourish.
We are profoundly grateful to our donors and partners who share our mission to advance health equity. We continue breaking down barriers to healthcare access while honoring each community’s unique strengths and experiences. Your generosity helps us reach children and families where they need us most, ensuring that every child, regardless of their ZIP code, has access to a healthy future. Together, we are creating lasting change.
Growing Stronger Together
 Children and families thrive best when healthcare and supportive services work in harmony rather than in siloes. The Stronger Together pilot project, led by the Schreiber Family Center for Early Childhood Health and Wellness team, leveraged the Magoon Institute’s programs to support leadership, teachers and families at Touch by an Angel®, an early childhood education center in Austin. The goals of the pilot were to improve early learning experiences and encourage healthy bodies, minds and families. Teams from our Food, Activity, and Nutrition (FAN) initiatives, Unintentional Injury Prevention and Maternal and Child Health initiatives provided leadership and teacher trainings. Lurie Children’s Center for Childhood Resilience (CCR) provided expertise on early childhood mental health, trauma and resilience.
Children and families thrive best when healthcare and supportive services work in harmony rather than in siloes. The Stronger Together pilot project, led by the Schreiber Family Center for Early Childhood Health and Wellness team, leveraged the Magoon Institute’s programs to support leadership, teachers and families at Touch by an Angel®, an early childhood education center in Austin. The goals of the pilot were to improve early learning experiences and encourage healthy bodies, minds and families. Teams from our Food, Activity, and Nutrition (FAN) initiatives, Unintentional Injury Prevention and Maternal and Child Health initiatives provided leadership and teacher trainings. Lurie Children’s Center for Childhood Resilience (CCR) provided expertise on early childhood mental health, trauma and resilience.
We provided six teacher trainings, identified caregiver needs and provided referrals to services.
Staff noted the trauma trainings were especially needed. Several parents who had children at the center had died in the past year. CCR’s trainings helped staff cope, support the families in their care and better understand how young children were processing loss.
We are expanding this program to additional licensed home- and center-based early childhood education providers in the coming year.
Supporting Healthy Beginnings
Every child deserves the best start in life. When families have access to the support they need, they can build a strong foundation for their children’s futures. Led by Katelyn Kanwischer, the Magoon Institute’s Maternal and Child Health initiatives – Connect Home Visiting Chicago (CHVC) and West Side Healthy Parents and Babies (WSHPB) – ensure more families receive necessary support, whether through home visits, support groups or connections to community-based resources. Our programs received 304 referrals last year and worked with 97 school and organizational partners to serve families.
Many organizations can only provide help once families are formally enrolled in a program. Our Parent Educators meet families where they are, providing whatever support is needed, from linking them to home visiting to helping fill out a housing form, creating an email address or simply being there in times of need. Families are empowered to choose the level of engagement that is right for them.
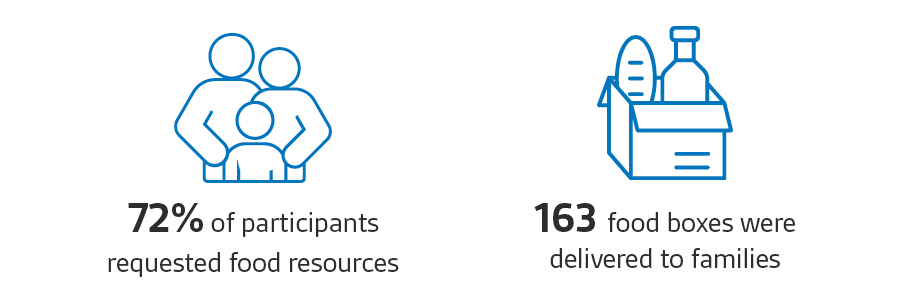
Over the past year, we have seen an increase in the complexity of the cases with families experiencing housing and food insecurity, interpersonal violence and other stressors, in addition to needing pre and postnatal care. Most families need several referrals and hours of support from our team. Yet, our commitment remains unwavering: to fill the gaps, provide a support system and ensure no family is left waiting.
Improving Sleep Safety

Dominique Johnson, Infant Safe Sleep Coordinator for Lurie Children’s Unintentional Injury Prevention Program, is a driving force behind the hospital’s focus on one of the most preventable causes of infant deaths: unsafe sleep environments. This work is especially urgent in Chicago, where Black infants are 14 times more likely to die from sleep-related causes compared to their white counterparts. Hispanic/Latinx infants in Cook County also face a risk 2.5 times higher than the national average, despite generally lower rates of infant mortality nationwide.
Advancing Food Equity
Our Food, Activity and Nutrition (FAN) initiatives team provides holistic, community-responsive programming, emphasizing food equity. Launched this year, the Vibrant Kids initiative led by FAN is aimed at curbing the disproportionately high rates of children diagnosed with Type 2 diabetes in Belmont Cragin. Families will receive one-on-one counseling, group lessons with a registered dietician and visits to neighborhood restaurants serving diabetes-friendly dishes. Hear more about how FAN is working with the local community to keep kids healthier in this segment that aired on WBEZ Chicago.
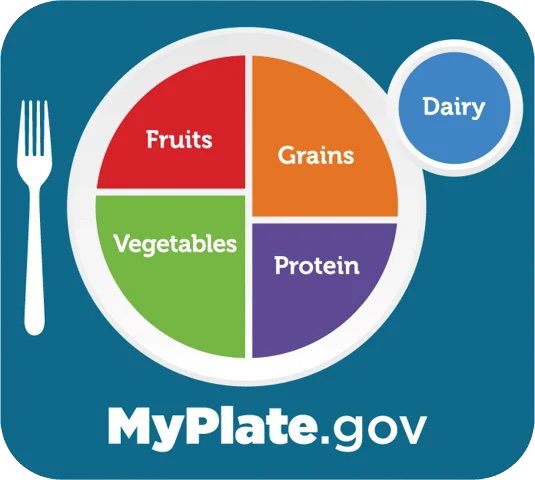 This year Lurie Children’s became the first children’s hospital in the Midwest, and the first specialty children’s hospital nationwide, to be named a MyPlate National Strategic Partner by the U.S. Department of Agriculture (USDA). This recognition highlights Lurie Children’s role as a key player in integrating nutrition into healthcare systems across the country and helping to shape policies that advance food security and health equity.
This year Lurie Children’s became the first children’s hospital in the Midwest, and the first specialty children’s hospital nationwide, to be named a MyPlate National Strategic Partner by the U.S. Department of Agriculture (USDA). This recognition highlights Lurie Children’s role as a key player in integrating nutrition into healthcare systems across the country and helping to shape policies that advance food security and health equity.
Building Hope on the West Side
Our work to develop the Austin HOPE Center continued this fall with a special youth engagement meeting. Young people from Lurie Children’s Adolescent Medicine program, KIPP Elementary, Boys and Girls Club and Communities United came together to learn how their input has shaped the project so far and to continue to share their ideas. The highlight of the event was a workshop with artist Jordan Campbell from Alt Space Chicago to help design the mural that will adorn the building.
Read more about our progress and watch a video of our groundbreaking here.

Disrupting the Cycle of Violence

Exposure to violence deeply impacts children, youth and their families. The trauma extends beyond physical injuries—affecting mental health, cognitive development and overall well-being.
A new initiative is underway to break the cycle of violence that brings children and their families into the Emergency Room. The Hospital-Based Violence Intervention Program (HVIP) offers immediate, compassionate support to young victims of violence and their families at a time when they are most vulnerable.
Bringing Care to the Community


By bringing our healthcare expertise to neighborhoods throughout Chicago, the Mobile Health Program maximizes the positive impact that Lurie Children’s can have on the health and well-being of children, youth and families. Now in its fifth year, the program is extending its reach through new partnerships and additional subspecialty services. In addition to providing school and sports physicals, immunizations well child visits, and sexual health education, the Mobile Health Program now operates four subspecialty clinics, focusing on high-risk asthma, weight and wellness and neurodevelopmental support for infants born prematurely or with cardiac conditions. Last year, these clinics served 150+ patients. Three more subspecialty services—cardiology, nephrology and endocrinology—are slated to begin offering mobile health clinics by the end of 2024.
Hear more from Jacinta L. Staples, DNP, MSN, BSN, BS, RN, Director, Community-Clinic Collaborations
Harnessing Youth Potential
Last year, our Mentorship and Workforce Development program served 573 students through 14 programs, introducing them to healthcare careers. Since 2021, 75 alumni have been hired at Lurie Children’s including Aniyah:
As a junior at Richard T. Crane Medical Preparatory Magnet High School, Aniyah participated in our Revenue Cycle Certification Program, which is offered in partnership with Rush University Medical Center. The program sparked her interest in healthcare and biomedical technology. While at the hospital during the summer program, Aniyah was very engaged and became especially interested in biology and engineering. This interest led her to placement in our biomedical equipment department with Healthcare Technology Manager Victor Rojo. The two formed a strong working relationship, and Victor ultimately offered Aniyah a job after she graduated high school. Aniyah now works full‐time at Lurie Children’s as an apprentice to become a biomedical equipment technician (BMET), a position she was introduced to through the Revenue Cycle Certification Program.
